Diabetic Wounds Differ from Regular Wounds
Diabetes significantly impairs the body's natural healing mechanisms and offers the ideal environment for infection to thrive. Diabetes-related blood glucose imbalances severely limit white blood cell activity. Without white blood cells to fight infection, germs can easily establish a foothold and spread across any incision, regardless of the initial size of the wound. Many of persons suffering from diabetes also experience impaired circulation, which exacerbates the situation further. Red blood cells are required to carry nutrients to the wound and cannot do so when circulation is not functioning as intended. As a result, this exposes the wound to infection and depletes it of the nutrients it requires to recover. The risks on developing complications from a non-healing wound increase significantly for those suffering from neuropathy as well, as the slow healing wound might be invisible to you and go undetected for weeks or months, due to a loss of feeling or sensation.

Why Choose Us for Diabetic Wound Care?
The Path to Successful Diabetic Wound Care
Checking your feet daily
Lowering blood sugar
Appropriate debridement of wounds
Treating any infection
Reducing friction and pressure
Restoring adequate blood flow

Keep Informed. Take Care.
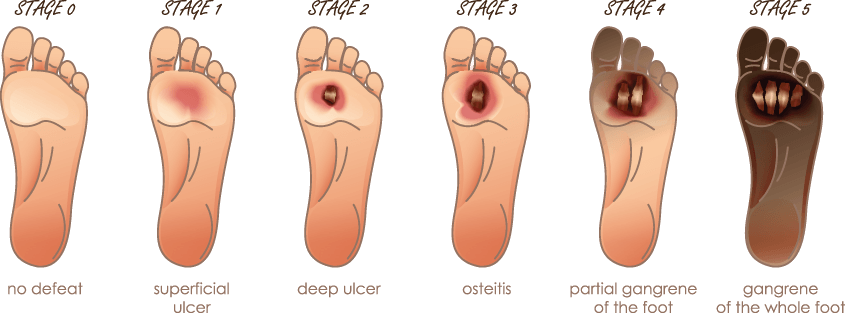
Each year, nearly half of diabetic patients with diabetic foot ulcers are hospitalized owing to serious complications, and nearly a quarter must have their limbs amputated. Diabetes is the primary cause of non-traumatic lower extremity amputation in the US.
Am I at Risk of a Diabetic Foot Ulcer?
You are at risk of developing a diabetic foot ulcer if you have or do any of the following:
Neuropathy
Poor Circulation
Foot Deformity
Uncontrolled Blood Sugar
History of previous foot ulcers
Inappropriate footwear